Creating Status Neutral HIV Prevention and Care
By Li Lock, PhD, MEd | June 16, 2023
Research Associate, ETR
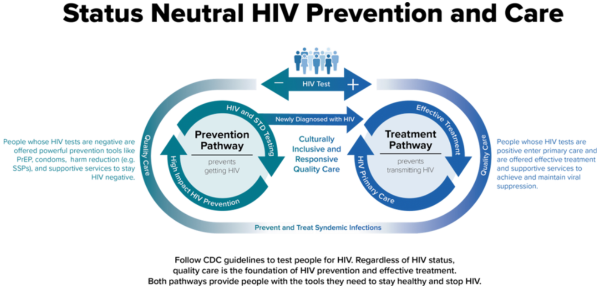
HIV services have historically been split into prevention (for people whose HIV test is nonreactive) and treatment (for people whose HIV test is reactive), often with additional services, such as primary care and housing, more readily available to those on the treatment side.
This has been due to a variety of factors, including the general availability of services, how funding streams to support HIV work have been organized, how staff are trained, and the stigma associated with HIV.
However, there’s a new concept emerging in HIV services that can help change the landscape of HIV prevention and care, as well as your direct work with your community: status neutral.
What Does “Status Neutral” Mean?
Simply put, a status neutral approach means the focus is on the person, and not their HIV status.
In a status neutral approach, all people are tested for HIV and offered effective prevention and/or treatment options. In addition, rather than letting HIV status dictate what services individuals are offered, all people are also connected with the services and support they want and need. Services address the social determinants of health, like access to stable and sufficient income, education, and healthcare.
When people’s needs are met, they are more likely to be successful in achieving their healthcare goals. This is why in a status neutral approach, all services and support are ultimately part of prevention.
Why a Status Neutral Approach?
Using a status-neutral approach makes a difference in the lived experiences of people seeking HIV services. Here are some ways that the status-neutral approach has the potential to have a positive impact in your community:
- Reduce HIV stigma: A status neutral approach centers the person rather than their HIV status. In doing so, we can rehumanize people with HIV and reduce HIV stigma. Discrimination and prejudice are impossible when we treat every member of the community with respect, compassion, and cultural humility.
- Make care more accessible: To be most effective, we must meet people where they are. In a status neutral system, services are provided in the places and ways that are best suited to the people they serve. For example, if a person needs mental health support, their level of service should be matched to their situation, whether monthly outpatient services would be best, more frequent home-based services, or something else. By eliciting their needs and matching services to meet those needs, we ensure that services are accessible to the people we serve.
- Facilitate optimal health: When people feel welcomed, respected, and comfortable, they are more likely to remain engaged in health and social service and support systems. Staying engaged with needed care and services over time can move people closer to optimal health and improve long-term results.
- Create more efficient service delivery: In a status neutral system, services are integrated and networked. Community members are connected with all the forms of care and support they want and need through in-house services and referral with a warm handoff. This ensures that the process of getting people connected with care is smoother and quicker than it otherwise would be.
- Result in greater health equity: Often times, people who belong to marginalized groups experience the greatest inequities in access to services as well as health outcomes. When services are accessible and provided in a culturally and linguistically sensitive way, people who experience the greatest health inequities are better positioned to stay healthy and well, ultimately eliminating those disparities.
By using this approach across HIV services, we can move closer to ending the HIV epidemic.
Creating Status Neutral Services
The status neutral approach to HIV services can be applied in many ways, such as: 
- Taking a person-centered approach to addressing health and wellbeing by assessing your needs and navigating you to meet those needs based on local services.
- Normalizing HIV testing, prevention, and treatment! Talk about it, get tested, and get connected with the care you want and need.
- Instead of focusing solely on disease prevention and treatment, focusing on health and well-being. There are so many ways to feel good and take care of our bodies, minds, and spirits in addition to any necessary treatment!
- Identifying where community members can access comprehensive services, like housing support, income stabilization, education and job training, primary medical care, mental health care, etc.
- Ensuring those services are available to everyone, regardless of HIV status.
Want to Learn More?
Review this issue brief on Status Neutral HIV Care and Service Delivery, and take the Status Neutral HIV Services course developed by ETR for free on CDCTRAIN in English or Spanish.
Dr. Li Lock (they/them/theirs) is a research associate at ETR and has worked as a sexuality researcher, program evaluator, and educator for the past decade. Li draws on their multidisciplinary background by applying systems theory and holistic models of sexuality to their work in sexual health and HIV prevention and treatment. Li can be reached at li.lock@etr.org.